Want to check if your trusted doctors are part of our PPO network? Simply search by inputting the zip code where you want to look for care and select “Blue Preferred” as your network.
This network contains both primary and specialty care providers to choose from. Members who are enrolled in County Employee Plan A, Plan A2T, Plan A2P, IHSS Plan and Senior Health Basic Plan must chose providers from this network only. Our Community Provider Network (CPN) is a network of community based private providers of primary. The Latino Providers Network manages and coordinates a membership community base umbrella organization with over 70 organizations and 200 individual members that provide direct services to the Latino community in the Baltimore Metropolitan Region in the areas of health, education, immigration, business, employment, arts & culture. Provider Network Overview GEHA's network of providers is one of the largest in the nation and includes more than 2.7 million in-network provider locations and over 9,300 hospitals. In-network cost savings Our fee-for-service plan offers services through a PPO. Bright Horizons Back-Up Care Advantage ® Provider Portal Welcome to the Bright Horizons/Back-Up Care Advantage® Online Provider Portal! If you have any questions or require assistance accessing the portal, please contact us at providerportalgroup@brighthorizons.com or contact the Provider Relations Team.
A World of Choices
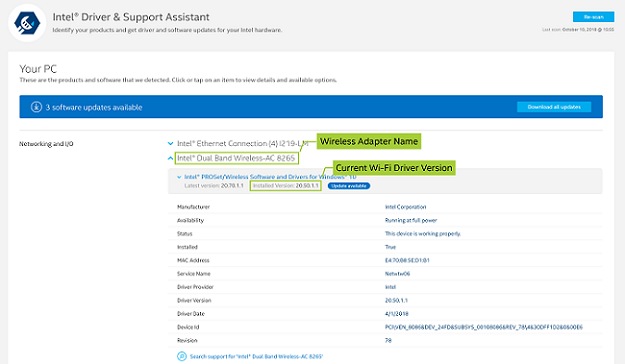
Provider Network & Wireless Cards Driver Download Windows 7
Your membership gives you a world of choices. Whether you need care here in the United States or abroad, you'll have access to health care in more than 190 countries.
With a provider network this comprehensive — more than 1 million physicians as well as provider facilities, hospitals and other care centers — most of your care needs are covered in-network, which means savings for you. Pentablet input devices driver.
Provider Network & Wireless Cards Driver Download Windows 10
Connecting You to the Best Care
For the best health, you need the best care that’s centered on your unique needs, delivered at the right place at the right time. CareFirst has programs which focus on the relationship between you and your doctor whether a physician or nurse practitioner. These programs provide your doctor with a more complete view of your health needs, enabling him/her to use this information to better manage and coordinate your care, a key to better health.

24/7 Care When Your Doctor is Unavailable
Free 24-Hour Nurse Advice Line
Call anytime to speak with a registered nurse. Nurses can provide you with medical advice and recommend the most appropriate care.
CareFirst Video Visit
See a doctor 24/7 without an appointment. You can consult with a board-certified doctor whenever you want on your smartphone, tablet or computer
Continuity of Care
If you are in the middle of treatment or the last trimester of pregnancy and your doctor doesn’t participate with CareFirst, you may be eligible for our Continuity of Care process. Skyhawke network & wireless cards driver download for windows 10. This process allows you or your dependents to receive care from out-of-network providers for up to 90 days. Complete the Continuity of Care form and submit it to CareFirst to determine if you qualify for this process.
Viewing and printing this document requires Adobe Acrobat Reader, which can be downloaded free from the Adobe site. Safa media driver download for windows 10 pro.
Nationwide, more than 96% of hospitals and 91% of professional providers contract directly with Blue Cross and Blue Shield companies.

1,006,430 physicians are in-network
NCQA Provider Network Accreditation creates a framework for organizations to provide efficient, accurate and consistent network management and credentialing services.
A QUALITY IMPROVEMENT FRAMEWORK
Many health insurers rely on tiered and narrow networks to manage costs, and use third-party organizations to validate their networks. In response to these network designs, states and the federal government implemented regulations requiring a minimum level of access to care and services.
The NCQA Provider Network Accreditation helps organizations maintain a high-quality network for members and clients by ensuring organizations:
- Ensure appropriate client agreements.
- Verify credentials.
- Protect credentialing information.
- Ensure credentials peer review process.
- Evaluate contracted provider quality.
- Monitor sanctions and complaints.
- Use objective evidence.
- Maintain adequate network.
- Provide access to appointments.
- Facilitate the continuity and coordination of care.
- Provide physician directories.

Get Started
We’re ready to help
Contact us today
